Sepsis
Since the first written account of sepsis in ancient Greece over 2,000 years ago, sepsis has challenged medical understanding for millennia. Etymologically derived from the Greek word “sepo” meaning “I rot”, sepsis was conceived as a putrefaction within a person’s body caused by an internal toxin or decay.
We now know that sepsis is a complex condition predicated by an underlying infection – bacterial, viral, or fungal – that provokes an exaggerated immune response from the host. The resulting hyperactive reaction causes a progressively toxic inflammatory cascade throughout the whole body that, without prompt treatment and control, can lead to severe organ damage and death. One of the most common causes of sepsis are bloodstream infections.
At a glance
It’s a killer
Dr Gorm Lisby, Chief Consultant, Amager and Hvidovre Hospital, Department of Clinical Microbiology, talks about how sepsis can affect anyone, at any time. But this is preventable.Shahrzad’s story
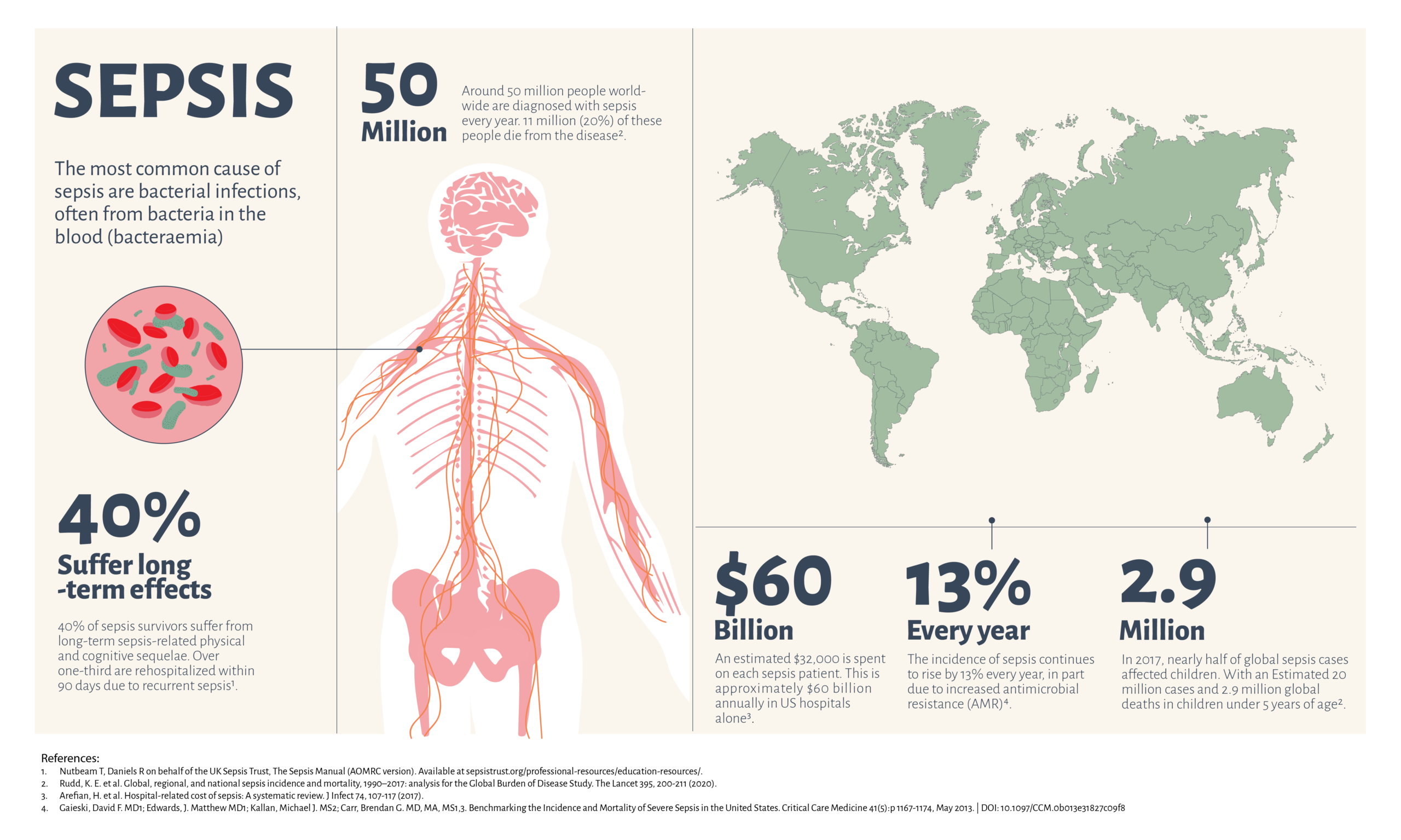
Shahrzad Kiavash is a sepsis survivor with an extraordinary story. Listen to her story here.Sepsis knows no borders and can affect anyone. An estimated 50 million people are afflicted by sepsis worldwide every year and over 11 million lose their lives to the condition. To put this into perspective, sepsis is responsible for 1 in 5 global deaths, more than cancer and HIV/AIDS combined. A number that is continuing to rise alongside the escalating threat of global antimicrobial resistance.
Time is key
Sepsis is a time-sensitive condition that demands immediate and correct antimicrobial treatments; the risk of mortality increases with each hour of delayed appropriate treatment. Without prompt intervention, sepsis can very rapidly escalate into septic shock, where mortality rates exceed 40%.
The cornerstone of effective patient care and survival hinges on patient response to empiric (broad spectrum) antimicrobial therapy. This non-targeted treatment is initiated at the onset of a suspected infection, and the timely availability of antimicrobial susceptibility testing (AST) results are necessary to refine treatment options through antimicrobial escalation, de-escalation, and dosage optimisation.
Unfortunately, the current standard of care methods for AST can take upwards of 48 hours, when time is a commodity that these patients do not have. This underscores the urgent need and unmet demand for rapid AST systems that can streamline the diagnostic workflow and help guide swift treatment decisions for the benefit of patients with bloodstream infections and sepsis.
Learn how ASTar can be part of the solution

For a list of sources cited on this page, click here