Antimicrobial resistance
Known as the “silent pandemic” antimicrobial resistance (AMR) has infiltrated every corner of the globe and threatens the continued effectiveness of antimicrobials.
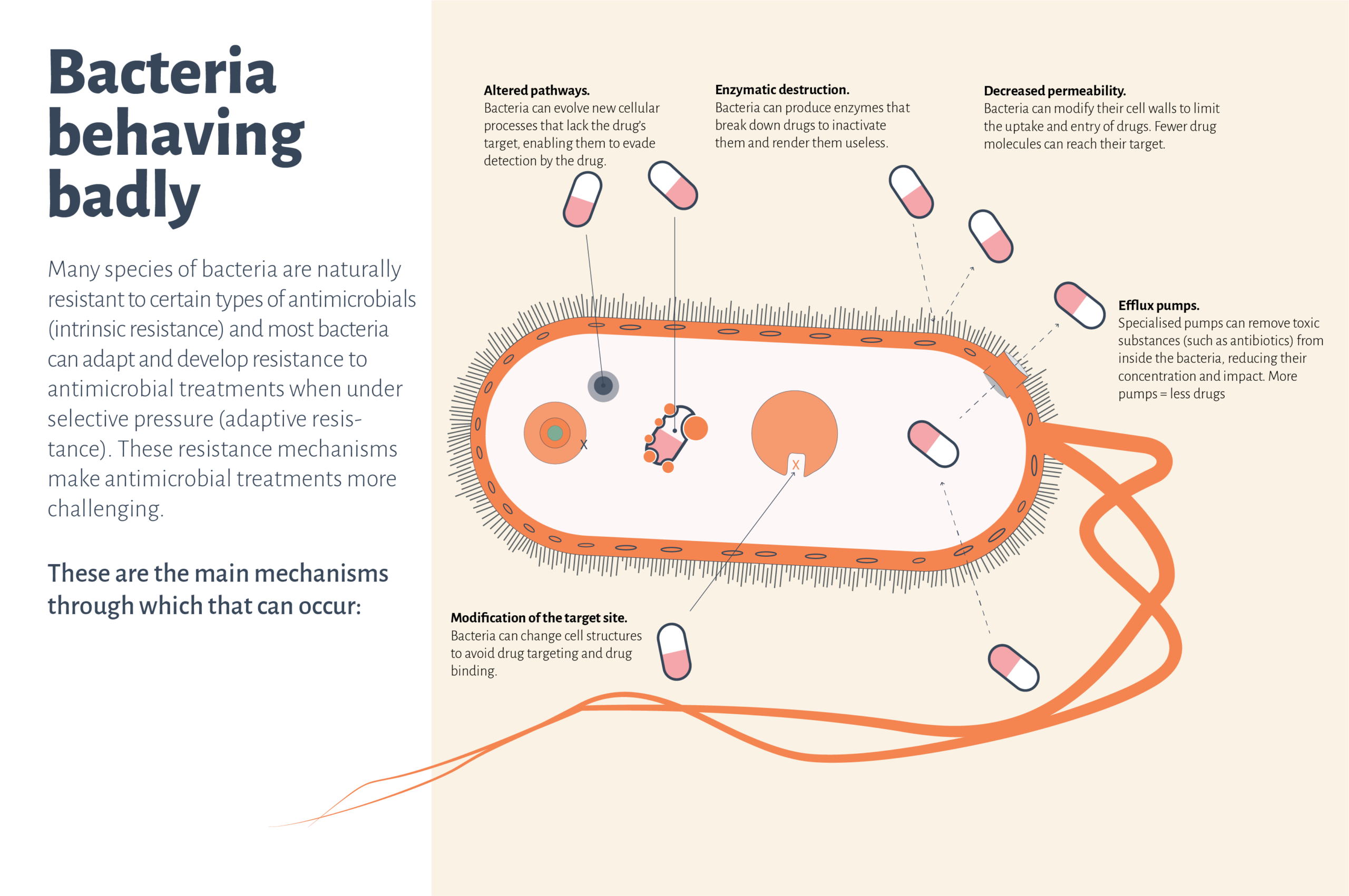
Antimicrobial resistance is the process by which pathogens stop responding to antimicrobial treatments that were previously working. A once easy-to-treat infection could escalate into something much more serious – posing not only individual concerns but also societal risks.
Colloquially called “superbugs”, these pathogens are much more challenging to manage and require the use of more potent antimicrobials, often referred to as “last resort” options, and there is no guarantee that further resistance will not emerge.
With every new development of resistance, the tug-of-war between effective and ineffective antimicrobial treatments is reset.
Antimicrobial Resistance – The need for rapid diagnostics
Jan Gorm Lisby, Chief Consultant, Amager and Hvidovre Hospital, Department of Clinical Microbiology, on antimicrobial resistance and the dilemma it presents to society and healthcare.Alexander Fleming and the discovery of antibiotics
In 1928 Alexander Fleming discovered penicillin and revolutionized medicine. Now however, the threat of antimicrobial resistance is a global concern.There are an estimated 5 million global deaths associated with bacterial AMR every year, a number that is predicted to double to over 10 million by the year 2050.
1 in 5 deaths from AMR are children under the age of five.
Fighting back with Antimicrobial Stewardship
When fighting a dangerous adversary, an equally formidable strike force is needed. In the battle against AMR, the formation and use of Antimicrobial Stewardship Programs (ASPs) is crucial. These initiatives are the concentrated efforts between clinicians, microbiologists, and clinical pharmacists that aim to reduce the unnecessary use of antimicrobials while simultaneously monitoring the threat of AMR on a local and global scale.
A primer for future care
It is not enough to create new classes of antimicrobials or to repurpose older compounds. Rapid diagnostic systems that can be seamlessly integrated into ASPs and the diagnostic workflow are crucial.
Faster AST technologies can shorten the time to optimal patient treatment and help prevent the emergence of individual and societal AMR by minimizing the use of broad-spectrum antimicrobials.
AST technologies must be easy to update and expand based on the ever-evolving requirements set by AMR and clinical demand. When the future is impossible to predict, drug panels and pathogen coverage must be readily adaptable, a feature that ASTar provides.
For a list of sources cited on this page, click here